
The insulin pump is used to automatically deliver basal insulin continuously, and bolus insulin at meal times by pressing the buttons. For correction, a blood glucose value can be entered into the pump to calculate the change needed to increase (bolus) or deny the quantity of insulin to bring the blood glucose level back to the target value.
In insulin-dependent persons, blood glucose levels have been roughly controlled using insulin alone. The number of grams of carbohydrate is estimated by measuring foods, and is then used to determine the amount of insulin necessary to cover the meal. A simple open-loop model is used: an insulin to carbohydrate ratio (adjusted based on past success) is multiplied by the grams of carbohydrates to calculate the units of insulin needed. That quantity of insulin is then adjusted based on a pre-meal blood glucose measurement (insulin added for a high blood sugar and insulin removed for a low blood sugar). Insulin is injected or infused under the skin, and enters the bloodstream in approximately 15 minutes. After the insulin has acted in the bloodstream, the blood glucose level can be tested again and then adjusted with injection of more insulin, or eating more carbohydrates, until balance is restored.
There are notable differences with insulin replacement compared to the function of pancreatic insulin delivery:
- the insulin dose is predicted based on measured food (where accuracy of measured carbohydrate is difficult) whereas pancreatic insulin is released in proportional response to actual blood glucose levels;
- pancreatic insulin is released into to the portal vein, where it flows almost directly to the liver, which is the major organ for storing glycogen (50% of insulin produced is used by the liver);
- pancreatic insulin is pulsatile which helps maintain the insulin sensitivity of hepatic tissues;
- injected insulin is delivered subcutaneously (under the skin) but not directly to the bloodstream, so there is a delay before injected insulin begins to reduce blood glucose (although this can be compensated by injecting insulin 15 minutes before eating);
- replacement insulin therapy does not include amylin (although Symlim is now available for use), which can reduce the insulin need by 50%;
- replacement insulin is dosed as a best compromise between aggressive use for lowering the blood sugar when eating but also conservative use to avoid a postprandial low blood sugar due to excess insulin, whereas pancreatic function releases insulin aggressively and later includes automatic release of glucagon at the end of an insulin cycle to manage the blood sugar level and avoid hypoglycemia.
An insulin pump to infuse a rapid-acting insulin is the first step in simulating the function of the pancreas. The pump can accurately deliver small increments of insulin compared to an injection, and its electronic controls permit shaping a bolus over time to match the insulin profile required for a given situation. However, the pump is still controlled manually by the pump user to bolus on command based on a snap shot of the recent blood glucose level and an estimate of the grams of carbohydrate consumed. This predictive approach is said to be open-loop. Once a bolus has been calculated and delivered, the pump continues to deliver its basal rate insulin in the manner that has been programmed into the pump controls based on the predicted insulin requirements of its user.
While insulin replacement is appreciated as a life saving therapy, its practical use in controlling blood glucose levels sufficiently to avoid the long term complications associated with hyperglycemia is not ideal.
Dosing[]

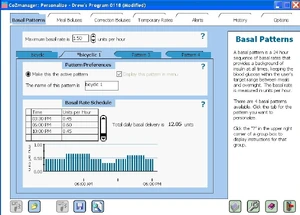
Customizing the basal rate pattern (units per hour) on an insulin pump
An insulin pump allows the replacement of slow-acting insulin for basal needs with a continuous infusion of rapid-acting insulin.
The insulin pump delivers a single type of fast-acting insulin in two ways:
- a bolus dose that is pumped to cover food eaten or to correct a high blood glucose level.
- a basal dose that is pumped continuously at an adjustable basal rate to deliver insulin needed between meals and at night.
Bolus Shaping[]
An insulin pump user has the ability to influence the profile of the rapid-acting insulin by shaping the bolus. While each user must experiment with bolus shapes to determine what is best for any given food, they can improve control of blood sugar by adapting the bolus shape to their needs.
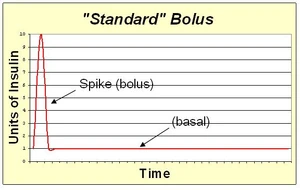
A standard bolus is an infusion of insulin pumped completely at the onset of the bolus. It is most similar to an injection. By pumping with a "spike" shape, the expected action is the fastest possible bolus for that type of insulin. The standard bolus is most appropriate when eating high carb low protein low fat meals because it will return blood sugar to normal levels quickly.
An extended bolus is a slow infusion of insulin spread out over time. By pumping with a "square wave" shape, the bolus avoids a high initial dose of insulin that may enter the blood and cause low blood sugar before digestion can facilitate sugar entering the blood. The extended bolus also extends the action of insulin well beyond that of the insulin alone. The extended bolus is appropriate when covering high fat high protein meals such as steak, which will be raising blood sugar for many hours past the onset of the bolus. The extended bolus is also useful for those with slow digestion (such as with gastroparesis or Coeliac disease).
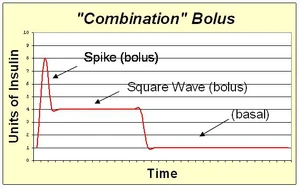
A combination bolus is the combination of a standard bolus spike with an extended bolus square wave. This shape provides a large dose of insulin up front, and then also extends the tail of the insulin action. The combination bolus is appropriate for high carb high fat meals such as pizza, pasta with heavy cream sauce, and chocolate cake.
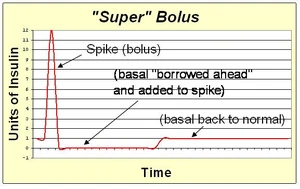
A super bolus is a method of increasing the spike of the standard bolus. Since the action of the bolus insulin in the blood stream will extend for several hours, the basal insulin could be stopped or reduced during this time. This facilitates the "borrowing" of the basal insulin and including it into the bolus spike to deliver the same total insulin with faster action than can be achieved with spike and basal rate together. The super bolus is useful for certain foods (like sugary breakfast cereals) which cause a large postprandial peak of blood sugar. It attacks the blood sugar peak with the fastest delivery of insulin that can be practically achieved by pumping.
Bolus Timing[]
Since the pump user is responsible to manually start a bolus, this provides an opportunity for the user to pre-bolus to improve upon the insulin pump's capability to prevent postprandial hyperglycemia. A prebolus is simply a bolus of insulin given before it is actually needed to cover carbohydrates eaten.
There are two situations where a prebolus is helpful:
- A prebolus of insulin will mitigate a spike in blood sugar that results from eating high glycemic foods. Infused insulin analogs such as NovoLog and Humalog typically begin to impact blood sugar levels 15 or 20 minutes after infusion. As a result, easily digested sugars often hit the bloodstream much faster than infused insulin intended to cover them, and the blood sugar level spikes upward as a result. If the bolus were to be infused 20 minutes before eating, then the prebolused insulin will be hitting the bloodstream simultaneously with the digested sugars to control the magnitude of the spike.
- A pre-bolus of insulin can also combine a meal bolus and a correction bolus when the blood sugar is above the target range before a meal. The timing of the bolus is a controllable variable to bring down the blood sugar level before eating again causes it to increase.
Both the blood sugar level as well as the type of food eaten have an impact on the ideal time to prebolus with the pump. New insulin analogs are "fast" enough to be given right before a meal, but this is ideal only when starting with a blood glucose value that is within range and the food to be eaten is of moderate glycemic index. If a time period of 15 or 20 minutes is considered to be a "time increment," then the prebolus time can be estimated by multiple increments. The time period is increased by one increment when blood glucose is high or when glycemic index is high. Time increments can also double, cancel, or go negative as the situation calls for as shown in the table below. Note however that an extended bolus allowed from the newer insulin pumps may be more convenient than a delayed standard bolus for a situation with low BG and low glycemic food to slow down the action of insulin.
| If The Blood Glucose Level Before Eating Is: | |||
|---|---|---|---|
| High GI Foods | Moderate GI Foods | Low GI Foods | |
| Above Target Range | 30-40 min before eating | 15-20 min before eating | 0-5 min before eating |
| Within Target Range | 15-20 min before eating | 0-5 min before eating | 15-20 min after eating |
| Below Target Range | 0-5 min before eating | 15-20 min after eating | 30-40 min after eating |
Basal Rate Patterns[]
The pattern for delivering basal insulin throughout the day can also be customized with a pattern to suit the pump user.
- A reduction of basal at night to prevent low blood sugar in infants and toddlers.
- An increase of basal at night to counteract high blood sugar levels due to growth hormone in teenagers.
- A predawn increase to prevent high blood sugar due to the dawn effect in adults and teens.
- In a proactive plan before regularly scheduled exercise times such as morning gym for elementary school children or after school basketball practice for high school children.
Basal Rate Determination[]
Basal insulin requirements will vary between individuals and periods of the day. The basal rate for a particular time period is determined by fasting while periodically evaluating the blood sugar level. Neither food nor bolus insulin must be taken for 4 hours prior to or during the evaluation period. If the blood sugar level changes dramatically during evaluation, then the basal rate can be adjusted to increase or decrease insulin delivery to keep the blood sugar level approximately steady.
Many factors can change insulin requirements and require an adjustment to the basal rate:
- continued beta cell death following diagnosis of type 1 diabetes (honeymoon period)
- growth spurts particularly during puberty
- weight gain or loss
- any drug treatment that affects insulin sensitivity (e.g. corticosteroids)
- eating, sleeping, or exercise routine changes
- whenever the control over hyperglycemia is degrading
- and according to the seasons.
Temporary Basal Rates[]
Since the basal insulin is provided as a rapid-acting insulin, the basal insulin can be immediately increased or decreased as needed with a temporary basal rate. Examples when this is helpful include:
- During a long car drive, when more insulin is needed due to inactivity.
- During and after spontaneous exercise or sports activities, when the body needs less insulin.
- During illness or stress, when basal demand increases due to insulin resistance.
- When blood ketones are present, when additional insulin is needed.
- During menses, when additional basal insulin is needed.